SALT LAKE CITY — One of the most common medical procedures in the country still comes with a long list of potential complications, but a group of students at the University of Utah is trying to cut that short, helping patients breathe easier.
A new device intends to make intubation safer for patients and more streamlined for professionals inserting the tube to open a person's airway.
"A lot of these complications are preventable," said Benjamin Fogg, a bioengineering and medical graduate student at the U. He said a lot of people have experienced complications from being intubated or know of someone who has.
Patients often have only minutes without oxygen before brain damage can occur, and intubation is the method physicians have of establishing an airway and utilizing a ventilator for a person who is not breathing on their own.
Complications resulting from poor intubation or multiple attempts to get the tubing inserted correctly can range from a sore throat to even death, Fogg said. The 29-year-old student and founding member of a medical device innovation company called Through the Cords has been working with Dr. Sean Runnels, an anesthesiologist at the U., and other students to develop a new endotracheal tube that makes it easier for medical professionals to perform endotracheal intubations.
Fogg is eyeing a career as an anesthesiologist and has practiced intubation on patients and says it is a nerve-wracking experience with "only a short amount of time to get it right."
"People only have three to five minutes before brain injury or death without oxygen," he said, adding that a large portion of the problem associated with intubation is "the inability to steer the tube into the airway."
More than 40 million intubations are done every year in the United States. It is done in the operating room for patients undergoing surgery. It is done throughout intensive care units and emergency departments on patients fighting for their lives. And it is done in a variety of settings by paramedics on rescue operations or in transit to medical care.
And of the many millions of intubations, about 400,000 require three or more attempts, according to research Fogg and his colleagues discovered while exploring and analyzing their up-and-coming medical device. And more than half of those die from not being able to breathe.
"It's a huge problem," Fogg said. "But it seems to be a preventable problem."
Physicians already have access to video laryngoscopy, which allows them to see where the tube is placed, but more than half of failed intubation procedures result from the tube landing in the wrong place.
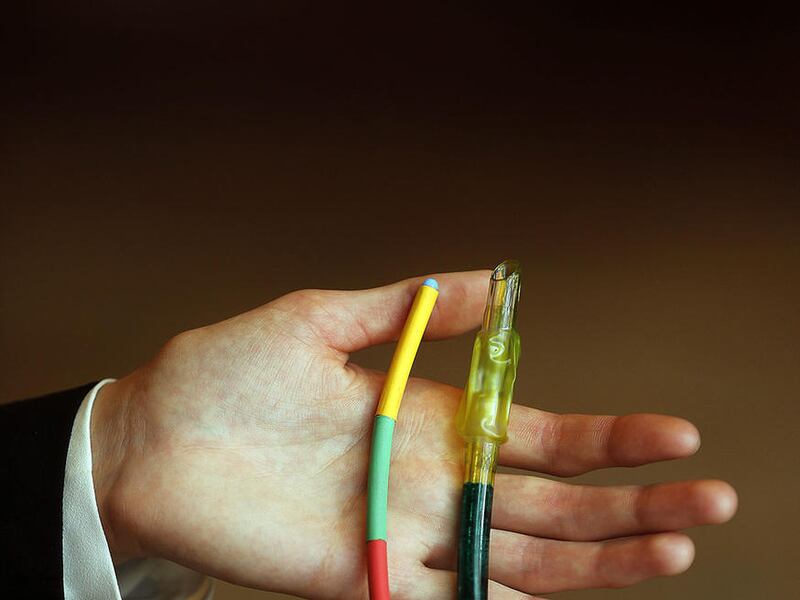
Through the Cords has developed a steerable introducer, which allows a provider to wind it into the windpipe correctly. A series of color-coded markers will tell them whether the tube has landed in a good spot — yellow indicates not far enough, green is a good position, and red means they've gone too far.
If a tube is inserted too deeply, Fogg said there is a risk of ventilating just one lung or puncturing it. And if it is placed too shallow, the patients won't get the oxygen they need.
Markings on current devices, mostly tiny numbers, are difficult to read from where it sits in the trachea.
Fogg said that perhaps the most encouraging feedback the team has received is that people who routinely perform intubation procedures have validated the need for a better product and see the device from Through the Cords as a perfect solution.
While the idea belongs to Runnels, the student-led group facilitated by the university's Lassonde Entrepreneur Institute has been able to run a market analysis and gather information about the common practice and how the device might be received.
The device has already won recognition from competitions and money prizes to further its development, and the students are committed to see it through approval by the U.S. Food and Drug Administration.
"It'll definitely save lives, no question," Fogg said. "It will prevent complications that are preventable. It will fix those problems and save lives."
Other members of the Through the Cords team include Mackenzie Hales, an MBA student, and Samer Merchant, a bioengineering student. Lassonde's New Venture Development program connects students from multiple disciplines to accomplish innovative projects like the new endotracheal tube.
Email: wleonard@deseretnews.com
Twitter: wendyleonards