SALT LAKE CITY — COVID-19 trends in Salt Lake County look positive, a testament to residents abiding by social distancing and protective policies set forth by local government and public health officials. But if residents grow weary and stop doing what they’re asked as restrictions begin to loosen, it could be disastrous, according to the Salt Lake County Health Department.
Friday, county public health officials briefed the Deseret News on what they’re seeing in terms of positive cases, hospitalizations, transmission rates and more.
Salt Lake County has been the hardest hit in Utah by the novel coronavirus, with 1,975 lab-confirmed cases (about 52% of the state’s total) as of Friday afternoon. Salt Lake County hospitals have treated 55% of the COVID-19 patients requiring that level of care. And 23 of 39 deaths in Utah — or 59% — have been there, as well.
But for folks weary of the restrictions imposed by the infectious respiratory disease, county officials point out good news that efforts to slow the spread are working:
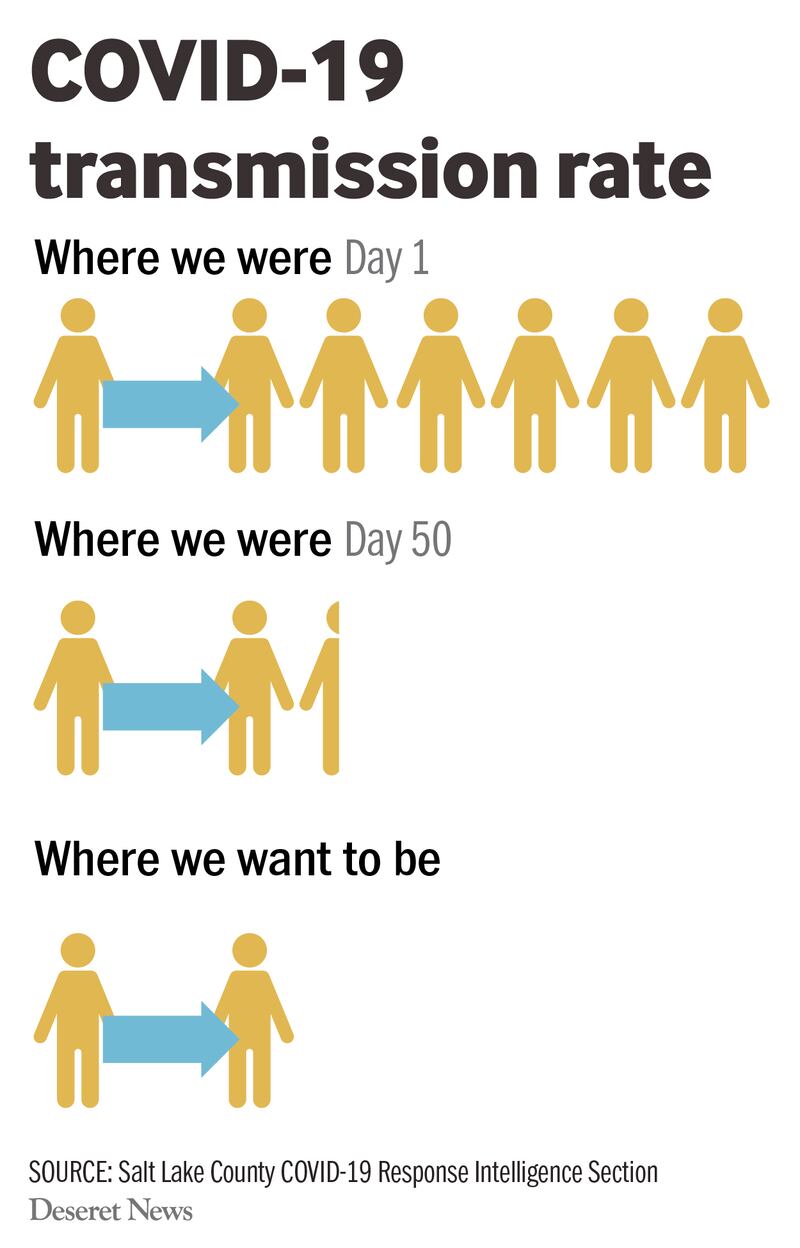
- The transmission rate has dropped dramatically. At the beginning of the pandemic, each positive person infected an average of six other people. That rate has dropped to an average of 1.3 infected by each.
“That is huge,” said Dr. Dagmar Vitek, Salt Lake County Health Department medical director, because each could infect six and it grows exponentially, with each of those infecting six more. “We would like it to be one person would only infect one person. We are almost there — absolutely amazing within 50 days.”
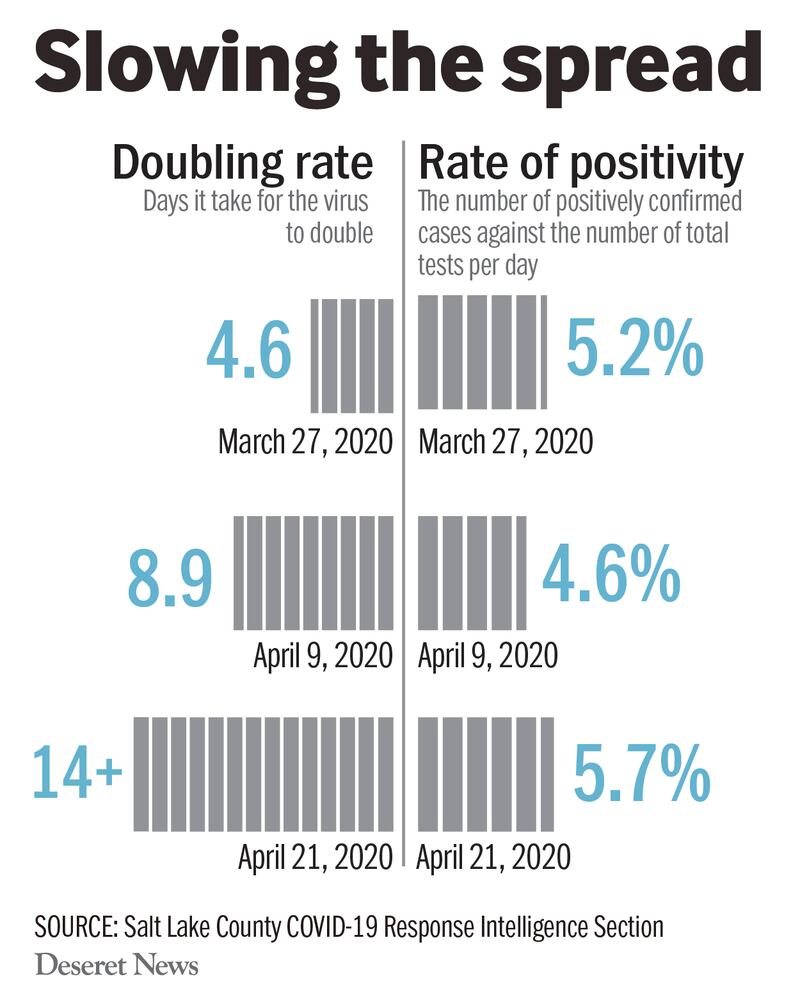
- On March 27, the number of infections was doubling every 4.7 days. By April 9, it took nearly nine days to double. On April 21, it took two weeks or more for cases to double.
- The county has conducted more than 33,000 tests for COVID-19 as of Friday.
- The number of positive tests compared to the total number of tests administered has consistently been in the range of 5%, which Vitek described as “fantastic” and much lower than in many other states.
- The county has reached nearly all the contacts of individuals with lab-confirmed virus, according to department spokesman Nicholas Rupp.
“We estimate we’ve been able to find the source of infection for about 85% of all Salt Lake County cases,” he said.
- Everyone worried that hospitals would be overrun. It hasn’t happened. Salt Lake County has been the busiest, but the hospitalization rate has been stable around 8%. By Friday afternoon, only 62 people were hospitalized for COVID-19 there.
And transfers to intensive care have been “steadily declining to below 50% now,” Vitek said. “Our hospitals are in great shape. That’s encouraging to see.”
“We have come a long way in these 50 days,” Vitek said. “I think it’s because of social distancing. We don’t have a vaccine and we don’t have any medication we can use, so the only measure we were left with is people staying home, people staying 6 feet apart, people wearing masks, people not gathering in parks or not partying, not going to movies. So obviously, whatever public health measures we implemented, they have all, combined, been extremely successful.
But she warned the urgency isn’t gone, as experts predict a second wave of infections next fall into winter. How large it will be depends on how patiently communities follow public health orders and practice good hygiene.
Testing
Testing has already given Salt Lake County and the rest of the state a pretty good idea of how many people are positive for the virus, according to Vitek, though people can be infected and not show symptoms. Even so, having many testing sites available to people with even very mild symptoms, combined with targeted testing whether people have symptoms or not, makes her confident “we are getting a good picture overall in Salt Lake County.”
When several people who are staying in a homeless shelter tested positive for COVID-19, county public health tested everyone in the shelters, separating those who are infected from those who are not. They have done the same thing at a residential drug treatment program and in long-term care facilities throughout the county.
Because it’s up to health care providers to refer people for testing and there’s some excess capacity, Vitek said she thinks some physicians may even be allowing some without symptoms to be tested, too, which bolsters belief that the county picture is accurate.
Salt Lake County would like to do more testing, including among Hispanics and people in some areas where testing has lagged a bit. Vitek said there may be some mistrust or misunderstanding about getting tested.
Contact tracing
Contact tracing has also clarified the degree of infections within the county. Staff have been brought in from other county divisions, including people who might normally monitor pollution or inspect businesses that are currently idled, to reach everyone an infected person might have exposed, going back two days before symptoms appeared.
“When we have a positive reported, we call and talk to them in person and gather all their contacts — family, friends, workplaces — then talk to all the contacts in person. So with 1,900 cases in Salt Lake County, we have probably talked to over 10,000 people who were contacts,” Vitek said
The county strongly recommends that all of those people who might be infected from an exposure to one who was infected get tested for the coronavirus, so that also catches people who don’t have symptoms. It would take 1.3 million tests to check everyone in the county.
While both Apple and Google have announced they’re developing apps to help with contact tracing, for the forseeable future Vitek believes the county will continue with the model it has in place, bolstered by some active monitoring tools from the Centers for Disease Control and Prevention and an app that Utah Gov. Gary Herbert’s office and state health officials worked on with developers.
“We have been very successful and I have to admit it has been brutal for our staff because we are working extremely long hours, but we are going to do what we need to do until this is over,” Vitek said.
Local and national experts agree it’s important to pace a return to normalcy carefully.
It is a “major risk” to reopen businesses and loosen other restrictions without extensive testing and contact tracing in each state, Dr. Crystal Watson, assistant professor at Johns Hopkins Bloomberg School of Public Health, said Friday in a national briefing.
Case-based interventions through extensive contact tracing will be needed in each community during reopenings. Watson said a “massive workforce upgrade” to contact tracing is needed nationally, along with more coordination between states and the federal government.
Challenges to contact-tracing include deciding which contacts are close enough to a case to be considered at risk. Many of those who test positive, are at-risk, or are awaiting test results face challenges to quarantining, including not having a place to stay. Public health must address those issues during the contact-tracing process, Watson said.
“This capacity is really needed to break those chains of transmission, but more importantly, at a population level, it’s to manage this epidemic on an ongoing, low level, in different places around the country. This will help us identify every case, or nearly every case, and stop them from transmitting to more people, and it will help us prevent future waves or surges of cases,” Watson said.
She called contact-tracing apps, like the one introduced this week in Utah, “a workforce multiplier” but said they won’t take over the role of public health workers.
A coming wave?
If a second wave occurs as predicted, it will arrive with the flu season and other respiratory illnesses. Sorting why people are sick will be trickier. Vitek predicts health care providers will have to do a lot of testing for both.
“I think we really need to push hard in the fall for everybody to get vaccinated for influenza so we keep those numbers down,” she added. “Hopefully by that time we could have a vaccine and maybe medications for coronavirus. That would help tremendously.”
To tame a second wave, restrictions have to be released slowly, health experts agree. If people start gathering in parks, eating out together, partying, returning to work and school without any social distancing, “I think the second wave would be horrendous. I think all of a sudden we would be in an accelerated phase again and see so many new cases.”
Officials have indicated a slow reopening of businesses and other aspects of normalcy. But people must mind those restrictions, she noted.
There’s no harm in being more cautious, but there’s a great deal of danger in flouting guidance.
“The bottom line is that I would love the public to listen to the governor’s and the mayors’ orders and follow them,” said Vitek. “If we relax the restrictions a little bit, go with that, but please stick to the ones that are in place.”
Contributing: Ashley Imlay



