- A mutated flu strain is causing efforts to heighten immunization awareness.
- A flu vaccine mismatch primarily concerns the A(H3N2) subclade K variant.
- Subclade K accounts for a third of confirmed flu cases in the U.S.
The holidays may spread a lot more than cheer this year. Think sniffles, headaches, exhaustion and a lingering cough. Influenza has made an earlier-than-usual debut this season and health officials are warning that a mutated strain of influenza, A(H3N2) subclade K, is spreading, which could mean a harsh flu season in the U.S., based on severe outbreaks elsewhere.
Dr. Robert Hopkins Jr., medical director for the National Foundation for Infectious Diseases, told Today.com that in Japan the variant has created “an unusually early and harsh flu season.”
And the British journal BMJ recently noted that the United Kingdom’s National Health Service is reporting “one of the worst winters ever,” largely because of concern over the mutated subclade K flu strain. Per the journal article, “Experts warn that the H3N2 strain, currently dominant in cases in England, mutated seven times over the summer, making it more severe than normal.”
Canadian scientists are also warning of mismatch between the updated flu vaccine and the subclade K strain, which is already circulating in most U.S. states, according to the Global Initiative on Sharing All Influenza Data. The Centers for Disease Control and Prevention say the little genetic changes have led to a “drift” from the version of A(H3N2) in the vaccine.
The World Health Organization reported that flu activity has ramped up globally and said that while the subclade K viruses circulating have several changes from other influenza A(H3N2) viruses, likely to boost its ability to spread, there’s no indication of an increase in disease severity. Still, the group notes “this subclade marks a notable evolution” from other H3N2 viruses.
Is it influenza?
In a season that can be crowded with respiratory symptoms — not just flu, but COVID-19 and respiratory syncytial virus, too — how can you recognize the flu?
It’s actually pretty easy, experts say, because of how abruptly it hits and how bad you feel. One minute you’re fine and the next you’re miserable, with symptoms that can include fever and chills, cough, sore throat, congestion, headaches, body aches and exhaustion. Sometimes the misery also includes nausea or vomiting, especially for children.
And while the flu itself typically resolves within a week absent major complications, the cough and tiredness can linger for weeks.
The Centers for Disease Control and Prevention estimated that as of Dec. 6, there have been “at least 2,900,000 illnesses, 30,000 hospitalizations, and 1,200 deaths from flu so far this season.” The CDC recommends both vaccination for anyone 6 months and older and use of prescription flu antiviral drugs should one get the flu, in order to lessen symptoms — especially for those at high risk of severe illness.
Of the flu types, H3N2 in all its variations is typically more severe than A(H1N1) or Influenza B — especially for older adults and young children.
“When we see early H3N2 activity, I think that’s particularly worrisome,” Andrew Pekosz, a virologist at Johns Hopkins University, told Today.com.
Subclade K here, there, everywhere
GISAID data show that subclade K has been found in 53 countries in the last four weeks and that in the U.S. it accounts for a third of confirmed flu cases. At least 30 states and the District of Columbia had reported cases of subclade K by the end of last week, the spread expected to continue.
The CDC surveillance reports have been lagging, the most recent dated Dec. 6. But it showed an upward trend for influenza in the U.S. and noted 6,884 patients had been admitted to hospitals that week for influenza. The health agency also reported that “among 163 influenza A(H3N2) viruses collected since Sept. 28, 2025, that underwent additional genetic characterization at CDC, 89% belonged to subclade K.”
CNN reported that most of the areas with a lot of flu activity right now are in the Northeast. “These include New York City, where activity is very high; New York and New Jersey, where it’s high; and Connecticut, Massachusetts and Rhode Island, which are in the moderate category. Flu activity is also high in Louisiana and Colorado. Other states and territories showing upticks are Georgia, South Carolina, Texas, Puerto Rico and Idaho.”
The CDC also reported the first death of a child from flu this season.
Advice to get vaccinated
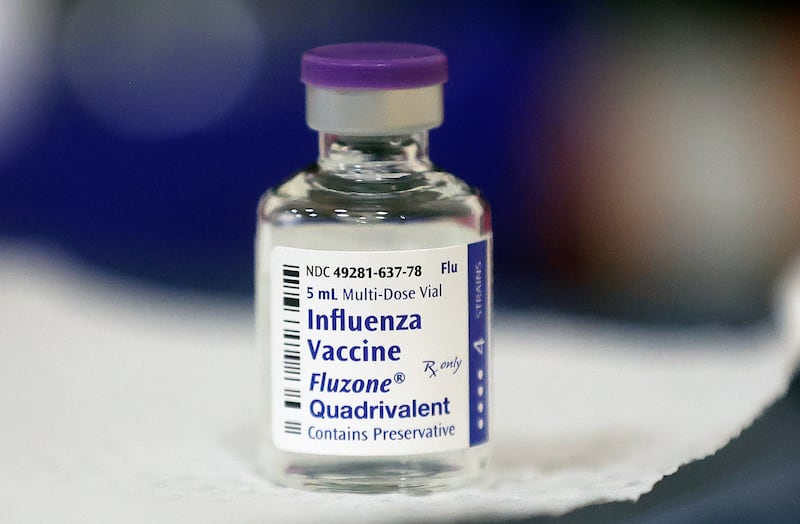
That the vaccine was prepared with other strains in mind doesn’t mean getting it isn’t helpful. Having a flu shot is expected to blunt the edges of illness enough to make it less likely either children or adults will become sick enough to be hospitalized or die. They will likely still show symptoms of the flu.
The CDC noted advantages to being vaccinated even if the match to what’s circulating isn’t perfect, including:
- Protection against severe illness, hospitalization and death
- Protection against other circulating influenza viruses that are in the vaccine
- Help to reduce overall community spread of flu
As Deseret News reported in November, low vaccine uptake also contributes to spread of flu.
Pamela Gomez, respiratory disease epidemiologist in the Utah Department of Health and Human Services, said then that people should still be vaccinated against the flu. “As soon as possible is the best action,” she told Deseret News, as even a less-than-perfect match will help keep those who get the flu from hospitalization. It should still reduce the severity should one be sickened by influenza.
While the vaccine’s makeup does not directly include subclade K, it does provide related influenza A protection, which should buffer some against subclade K’s severity were someone to become infected. And subclade K will not be the only flu variant to which people are apt to be exposed this winter.
Predicting flu season
What is expected and what actually happens don’t always line up, however. As CNN pointed out, “There’s an old joke public health veterans tell about the unpredictability of flu season: ‘If you’ve seen one flu season, you’ve seen one flu season.’ Some experts caution that the U.S. may not see the kind of activity as in other countries.”
Some experts believe that it’s not common to have two bad flu seasons in a row and last year’s was rough. “It’s not typical that you have two back-to-back bad flu seasons,” Dr. Jennifer Nuzzo, director of the Pandemic Center at Brown University, told CNN. “I have wondered if perhaps we might be somewhat more protected than some of these other countries because of what happened in the U.S. last year.”
Others believe the new variant and how quickly it mutates could quell that hope.