SALT LAKE CITY — Hospital officials again called on residents to work to stem the spread of COVID-19 on Monday even as one southern Utah hospital opened a “surge” intensive care unit to treat increasing numbers of coronavirus patients.
“We continue to see high volumes of patients in intensive care units at our hospitals across the state. New cases of COVID-19 and subsequent hospitalizations of COVID patients continue to spike in Utah,” Jess Gomez, spokesman with Intermountain Healthcare, said in a statement.
Statewide, 288 patients were hospitalized with the disease in Utah on Monday — three fewer than were hospitalized on Sunday. Overall intensive care usage again fell slightly to 69.7%, and nonintensive care unit usage fell to 48.3%. Officials last week warned intensive care usage of 75% or higher is unsustainable and could lead to patients not receiving the ideal level of care.
Just over 100 COVID-19 patients are in some of the state’s 600 intensive care unit beds, according to the Utah Department of Health. But bed counts provide an incomplete picture of hospital capacity in Utah, as patients in rural areas often need to be transferred to hospitals in nearby larger cities, where providers have the expertise to care for them.
Late last week, University of Utah Health also needed to open a surge intensive care unit to treat an influx of COVID-19 patients. On Friday, the hospital ran at 104% its intensive care capacity before use dipped overnight, hospital officials said.
On Monday, the hospital’s intensive care units were at 81% capacity, said Kathy Wilets, spokeswoman with U. Health.
“But I need to clarify that this number is still high. Our ICU bed rate includes both our surgical intensive care unit (non-COVID-19 patients) and our medical intensive care unit (includes COVID-19 patients). We typically dip down on the weekends because we aren’t doing as many surgeries. Our rate changes by the hour/day and it is expected to rise again this week,” she said.
“This is based on projections that include positive testing trends and the current hospitalization rate (some hospitalized patients move into the [medical intensive care unit] as they become sicker). I’d also note that we have some very time sensitive surgeries that need to take place this week that will also require ICU beds,” Wilets added.
Record hospitalizations
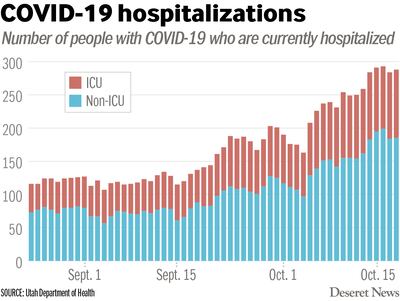
Throughout the state, COVID-19 hospitalizations remain in record territory.
Since the Utah Department of Health began releasing current hospitalizations in addition to cumulative hospitalizations in May, current COVID-19 hospitalizations only reached as high as 225 for one day in late July. For most of the pandemic, they lingered around the mid-100s.
Hospitalizations began to climb at the end of September and beginning of October about three weeks into the current surge. For the past eight days, they’ve been above 240.
During June, daily hospital admissions on average ranged between 10 and 30. In September, they’ve ranged between 30 and 50 each day, according to state health department data.
On Monday, health officials reported 1,168 new COVID-19 cases and three additional deaths, marking the sixth day in the row with more than 1,000 additional cases confirmed in the state.
Intermountain Dixie Regional Medical Center — the largest in the southern Utah region —has opened a surge unit due to “the rising number of patients requiring ICU care, including those with COVID-19,” Gomez said.
“This is part of Dixie’s surge plan to care for the increasing number of patients in the community who need high-level ICU care. Health care resources across the state, including highly trained caregivers who provide specialized intensive care, continue to be stretched due to the rising numbers of COVID-19 patients and subsequent hospitalizations,” Gomez said.
But intensive care units also need to treat non-coronavirus patients, he noted.
“We call upon the community to stand with us at this time: Please mask up, social distance appropriately, wash hands often, and stay home if sick. Our caregivers and patients throughout the community need your support to reduce transmission of this virus,” Gomez said.
Meanwhile on Monday, the overflow makeshift hospital at the Mountain America Expo Center had not been rebuilt — and officials do not expect to put it back up this week, said Joe Dougherty, spokesman with the Division of Emergency Management.
The makeshift hospital would only be put to use should hospitals request it, he said. If the need arises, officials will set it up three days before patients would get transferred there. Two semitrailers filled with supplies remain on site at the expo center, and two more semitrailers are loaded at the Utah Department of Health and ready to be transferred quickly.
The option is still, however, seen as a last resort. Before it happens, hospitals need to perform load-leveling within their own systems — transferring patients between hospitals to address capacity — and sharing the burden outside their own systems. The state also has contracts with three long-term care facilities to treat COVID-19 patients. Those facilities still had capacity as of Monday, Dougherty said.
At MountainStar Healthcare, another of the state’s larger hospital systems, intensive care units are far under capacity compared to others at about 65%, said Dr. Mike Baumann, MountainStar chief medical officer. The system has just 13 COVID-19 patients in intensive care, he said.

It’s typical for the system to be at lower capacity than University of Utah Health, as people often get referred there from other states, and Intermountain due to referral patterns and insurance programs, Baumann said.
He said officials with all the state’s major health care systems meet for weekly and biweekly conversations about load-leveling and how they can respond together to the surge — and that they’ve been prepared.
Despite MountainStar Healthcare’s strong capacity, Baumann said rising hospitalizations are still a “true issue” in the state.
“I think this is something that we really do need to be concerned about, seeing the increasing number,” Baumann said.“But the key is be prepared, be respectful, and the last thing, we need to do the basics. Masking, social distancing, hand hygiene, and not getting into large crowds,” he said.
Dougherty said it’s more important than ever to wear masks in social settings, even around family members, and to keep gathering sizes at no more than 10 people.
“We can’t have any more spread of the disease,” Dougherty said.
Data shows that more Utahns might now be wearing masks in public even before Gov. Gary Herbert last week announced increased restrictions, including a mask mandate for public events.
For the week ending Oct. 11, 99% of residents across Utah wore masks indoors in public locations where physical distancing is not possible, according to observational and survey data from the state health department.
Monday’s 1,168 cases were reported out of 6,721 tests, a 17.4% positive rate, according to the Utah Department of Health. The rolling seven-day average for new cases is 1,233 per day, and the average positive test rate is 14.4%.
The deaths reported Monday bring the state’s toll due to the coronavirus to 546. They were a Salt Lake County man between 45 and 64, a Utah County man older than 85, and a Washington County man older than 85, all of whom were long-term care residents.
Now 95,562 cases have been confirmed out of 980,659 people tested in Utah since the pandemic began, an overall positive rate of 9.7%. Just over 71,000 of the state’s cases are considered recovered after surviving the three-week point since their diagnoses. Hospitalizations since the outbreak began in Utah now total 4,688.
New COVID-19 cases reported Monday by health district:
- Salt Lake County, 500.
- Utah County, 330.
- Davis County, 93.
- Bear River, 69.
- Weber-Morgan, 60.
- Southwest Utah, 51.
- Tooele County, 23.
- Central Utah, 14.
- Summit County, 9.
- Wasatch County, 7.
- San Juan County, 5.
- TriCounty (Uinta Basin), 4.
- Southeast Utah, 3.


