After a year that claimed the lives of more than 300,000 Americans, including 1,148 Utahns due to COVID-19, hope came this week as the first vaccine made its way to health care workers across the country.
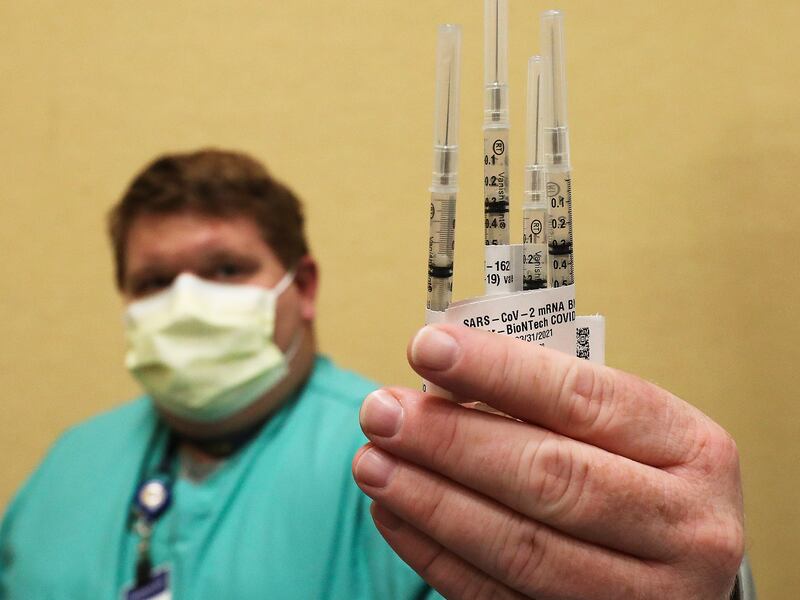
The FDA and CDC issued emergency use authorization for Pfizer/BioNTech’s vaccine late last week, the result of an accelerated vaccine development and approval process. The company says it shipped out 2.9 million doses this week.
Moderna’s vaccine received emergency use approval from the FDA on Friday and the Centers for Disease Control’s Advisory Committee on Immunization and Practices voted Saturday to recommend the vaccine for people 18 and older. CDC Director Dr. Robert Redfield must accept the recommendation, which is expected.
Last month, Pfizer and BioNTech announced their mRNA vaccine showed more than 90% efficacy, while Moderna announced its mRNA vaccine shows a 94.5% efficacy rate.
Both the Moderna and Pfizer/BioNTech vaccines require a second dose after 21 days.
Through Operation Warp Speed, the U.S. government expects to distribute 20 million vaccine doses by the end of December, said Gus Perna, chief operating officer for Operation Warp Speed, during a news conference Saturday.
Here’s a look at what we know now:
Does it matter which vaccine you receive?
According to the World Health Organization, there are more than 200 COVID-19 vaccines in development worldwide. National Geographic reported that the vaccines “involve eight different technology platforms, from innovative ones made of genetic material, such as DNA or messenger RNA, to classic varieties built from inactivated versions of the coronavirus.”
With two immediately soon to be available in America, health officials said both the vaccines — Pfizer’s or Moderna’s — have outstanding efficacy rates and will provide protection. Adding the Moderna vaccine will enable far more people to be vaccinated because unlike the Pfizer vaccine, it can be stored at normal freezer temperatures.
Who gets vaccinated?
Across the United States, front-line hospital workers are at the top of the list and began getting vaccinations last week. Nursing home residents and staff are expected to begin getting vaccinated in Utah around the end of December, followed in January by first responders, K-12 teachers and school staff.
Utah’s first vaccine doses arrived on Monday at two Intermountain Healthcare hospitals, and the immunization of the most at-risk front-line health care workers there and at University of Utah Health began a day later.
As of Friday, 14,625 doses of Pfizer’s vaccine had been shipped to the Beehive State. Intermountain Healthcare had vaccinated 2,300 health care workers, and University of Utah Health administered 1,500 vaccines to its workers, with another 1,000 planned on Friday, according to hospital leaders.
In February and March, vaccinations are scheduled for long-term care facility staff and residents who have not already been vaccinated.
From March through July, Utah’s vaccination plan will prioritize tribal reservation communities, residents ages 65 and older, employees in higher risk professions (like child care and airline workers), racial and ethnic groups at higher risk, workers in food preparation, and those with underlying medical conditions.
When can I get vaccinated?
The vaccine will be distributed to the general public only after the categories that are considered more at-risk, meaning it likely won’t be available to the general public in Utah until April.
Dr. Angela Dunn, epidemiologist with the Utah Department of Health, said last week it likely will be “late summer before we can have confidence that a vast majority of Utahns have taken the vaccine and we can rely on herd immunity.”
She urged Utahns to “continue being vigilant” by taking measures to stem the virus spread, and not let down their guard due to the vaccine becoming available.
Salt Lake, Utah’s most populous county, which has also been most hard-hit by deaths and hospitalizations throughout the pandemic, will take an all-hands-on-deck approach in administering the vaccine.
Any health professional with the ability “to put a needle in someone’s arm because they’re trained or authorized to do so” will be needed to administer the vaccine in the county,” said Salt Lake County Mayor Jenny Wilson.
Vaccinating the whole county will prove a challenge, the details of which are still being worked out.
“We have a lot of work to do, but we want to be doing as much as we logistically can. There are barriers, staffing shortages for certain folks and a need in hospitals,” Wilson said.
Will the vaccine be free to recipients?
Yes. Because the vaccine doses are purchased with tax dollars by the federal government, they are free to recipients. But providers may charge administration fees, which could be reimbursed by patients’ insurance companies, according to the Centers for Disease Control and Prevention. The Health Resources and Services Administration’s Provider Relief Fund will reimburse health care providers for uninsured patient vaccinations.
How many people need to get vaccinated?
Utah health care leaders have estimated it will be between April and July when vaccines become available to enough of the population to reach the 70% threshold for herd immunity and stop the virus from spreading.
That means more than 2.2 million people in Utah will need to get vaccinated to reach that level. Leaders, however, face the challenge of increasing confidence around the vaccine to get there.
According to a Pew Research survey conducted in September, about half of Americans (51%) said they would “definitely or probably” get vaccinated. The percentage of people who intend to get vaccinated fell sharply throughout the year from 72% in May, Pew researchers said.
About three-quarters of Americans (77%) responded that they believed a vaccine would get approved by the U.S. before its safety is “fully understood,” according to the study.
Is it safe?
Both Moderna’s and Pfizer/BioNTech’s vaccines contain a genetic material called mRNA that causes one’s body to trigger an immune response against SARS-CoV-2. Unlike flu vaccines, they don’t contain live or dead coronavirus and cannot give someone the infection.
According to the FDA, the Pfizer/BioNTech vaccine’s “known and potential benefits outweigh the known and potential risks,” and the safety of the vaccine has been thoroughly evaluated. The FDA recommended the vaccine be given to anyone 16 years or older. The use of the vaccine is given under emergency protocols, meaning intensive followup continues.
Reports out of Alaska of three health care workers having reactions to the vaccine should not dissuade one from taking the vaccine as protocols were followed and reactions of some kind are expected, health officials said; patients receive immediate care as part of the protocol.
While Moderna’s vaccine will not give you COVID-19 — and no serious side effects have been noted — some have reported mild to moderate effects following vaccination, including injection site pain, fatigue, muscle pain, joint pain and headache, according to Moderna.
Likewise, the most common side effects of Pfizer/BioNTech’s vaccine are fatigue, headache, muscle pain and chills — and they were more commonly reported following the second dose. People ages 16 to 55 were also more likely to report responses to the vaccine than individuals older than 55.
Little research has so far looked into whether or not the vaccine is safe for children and pregnant or breastfeeding women. Pfizer indicated last week that it is currently enrolling 12- to 15-year-olds in another study with a goal of enrolling 2,000. The company will then reportedly study dosing for 5- to 11-year-olds.
The U.S. Advisory Committee on Immunization Practice last week recommended that a pregnant woman be allowed to choose if she wants to receive a COVID-19 vaccine, and encouraged her to talk with her health care provider about it.
A woman should weigh the issues of COVID-19 spread in her community and her potential risks of contracting COVID-19 and the potential for personal complications or preterm birth, with the fact that there is no data yet on Pfizer/BioNTech vaccine use in pregnant women, the advisory committee advised.