SALT LAKE CITY — In the three days since Gov. Gary Herbert and other state officials announced the arrival of COVID-19 in Utah, hospitals across the state have ramped up preventive measures to combat a potential outbreak.
Over the course of a week, the University of Utah Hospital set up massive Blu-Med field hospital tents to test patients without exposing the hospital’s staff or patients; Intermountain Healthcare imposed new visitor restrictions; and MountainStar health rolled out a new screening process for patients and hospital visitors.
Philip Chaffee, director of emergency management at the University of Utah Hospital, says COVID-19 is not something Utahns should be afraid of.
“We have a plan, we are prepared, and they should feel a level of comfort knowing that we’re not waiting for things to happen,” Chaffee said, speaking from one of the Blu-Med tents, a 25-by-75-foot structure that can withstand 100 mph winds.
Although the tent was empty Monday, Chaffee said in a moment’s notice hospital staff can bring in computers and other medical equipment.
“In about 30 minutes we’re operational,” he said, “We’re positioned and able to surge and manage whatever does come our way.”

State officials launched coronavirus.utah.gov to keep Utahns up to date with all things COVID-19, including how to self-report. Anyone thinking they may have COVID-19 should call 1-800-457-7707, the state’s coronavirus line.
The Deseret News reached out to the Utah Department of Health for more information, but an official was not immediately available.
Health officials are urging anyone with COVID-19 symptoms — fever, cough and shortness of breath — to call the hotline or a health care provider rather than visit a clinic or hospital in person. Unless symptoms are severe, Utahns should fight COVID-19 from home.
“The vast majority of people who come into contact with this may not get symptoms at all or will get very mild respiratory symptoms that just caring for themselves — rest, fluids and comfort measures — will take care of,” said Dr. Shannon Phillips, chief patient experience officer and interim chief medical officer for community-based care at Intermountain Healthcare.
Best-case scenario? Tracey Nixon, chief nursing officer at the University of Utah Hospital, hopes Utah’s one reported case of COVID-19 stays contained in Davis County and doesn’t spread.
But that probably won’t happen, she acknowledged.
“If you watch what's happening across the nation, what's happened across the world, you can see that it spreads pretty quickly and fairly easily,” Nixon said.






Herbert announced the first case of COVID-19 in Utah in a Friday night news conference, hours after declaring a preemptive state of emergency. The patient, a Davis County resident, is believed to have caught the virus aboard the Grand Princess cruise ship, according to the state epidemiologist Dr. Angela Dunn.
On Monday, Lt. Gov. Spencer Cox confirmed the patient attended a BYU basketball game in February. As a precaution, BYU is contacting anyone sitting within 6 feet of the individual, according to a statement issued Monday afternoon.
At Friday’s press conference, Dunn and other officials said the patient is quarantined in their home and complying with an isolation order. But hospitals across Utah are not taking any chances.
Intermountain Healthcare is attempting to curb the potential spread of COVID-19 by only allowing two visitors per patient — in the case that a patient tests positive, hospital staff will isolate the individual.
Phillips also said Utah’s response to the virus hinges on the health of medical workers.
“Taking care of our caregivers is almost a primary importance,” Phillips said. “If we don’t have them, we can’t care for our communities as people get ill.”
With hospitals and clinics across the state, Phillips said rural locations pose a unique set of complications for Intermountain.
“If we lose health care workers at a rural facility we can certainly help them through the larger Intermountain system, but that stops us from serving our community,” said Phillips, noting that making sure caregivers are comfortable and competent with using personal protective equipment — hazmat-like suits straight out of Michael Crichton’s “Andromeda Strain” — is critical to ensuring rural clinics are fully staffed.
Phillips said Intermountain’s rural strategy is still a work in progress, and will likely be handled on a case-by-case basis. If the virus spreads, it’s possible infected patients will be transported and quarantined at a different, more centralized location.

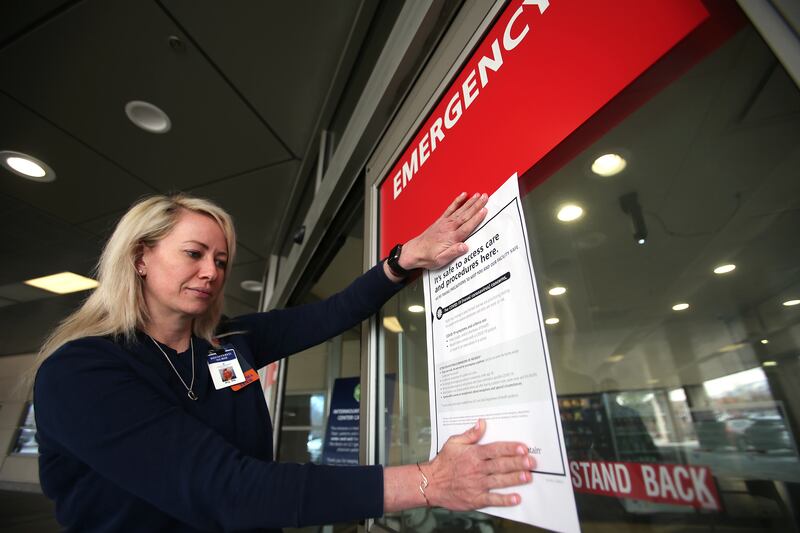
MountainStar Healthcare, which operates eight hospitals along the Wasatch Front, implemented a new screening process before Herbert’s announcement on Friday.
Now, any new patients or visitors will be screened for symptoms and asked if they’ve been to any areas with a high prevalence of COVID-19.
“If they answer yes to any of those, we ask them politely not to come into our facility so we can be sure to provide good health care without exposing other members of our staff or patients,” said Michael Baumann, MountainStar’s chief medical officer.
Baumann has a clear message for Utahns: “Have respect for what is going on, but don’t overreact,” he said. “As we find out more information we might actually need to be more concerned, but right now we just need to be sure we’re careful and have the proper systems set up.”
“No one should get hysterical or alarmed,” said Phillips, echoing Baumann and other health experts in Utah. “Most are going to do extremely well, and for those of us whose family members are a little older or a bit more frail, let’s care for them and keep them close to home and checked in on.”