SALT LAKE CITY — Though the week has started with lower-than-average new COVID-19 cases in Utah, a university epidemiologist said Tuesday the state still has work to do to meet Gov. Gary Herbert’s 500-case average by Saturday.
“It’s way too soon to know if the whole week will be low or if it means that when people get back from the long weekend and start to go in and get tested, we’ll see a big jump like we saw after the 4th of July,” said Lindsay Keegan, epidemiologist with University of Utah Health who leads the university’s team working on COVID-19 projections.
The Pioneer Day weekend likely impacted testing numbers, which affected new case counts due to reporting delays, Keegan said.
“When you look at the report date, you’re looking at variability based on labs open — on weekends we know some labs aren’t reporting, and we know that there’s some variability on when people are getting tested, backlogs that have to be filled,” Keegan noted.
News reports and daily updates from the Utah Department of Health emphasize new cases reported to the department that day. Tests results typically do not get reported on the day the tests are given; therefore, the new cases reported each day include results from tests performed between one and three days previously.
University of Utah epidemiologists focus on a different figure — the number of tests and positives from tests performed on a specific day. That data takes a few days to backfill on the Utah Department of Health’s coronavirus dashboard in a chart titled “Number of People Tested by Date.”
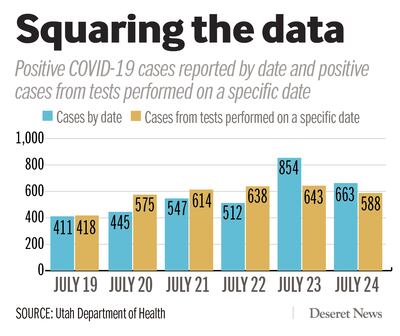
For example, on Thursday, 854 cases were reported to the health department, which included results from previous days that hadn’t yet made their way into the state’s tally. But tests that were actually administered on Thursday included just 643 positives.
According to that data, on Friday — the most recent day for which data has backfilled — 588 of 6,166 tested positive for the coronavirus. The previous four days brought cases in the mid-500s to mid-600s. Based on those numbers, Utah needs to see between 175 and 235 fewer positive cases each day to reach Herbert’s goal of a rolling average lower than 500, Keegan said.
On Tuesday, the rolling seven-day average for positive tests was 541 per day, and the positive rate of tests is 9.7%.
That average has continued to steadily decrease for the past two weeks.
On July 24, the state’s seven-day rolling average was 614 new cases per day, and percentage of positive tests was 9.1%. Just a week before that, on July 17, the rolling seven-day average was 699 cases per day, and positive tests were 10.3%.
The numbers have slowly started to flatten due to Salt Lake County’s mask mandate, Keegan said.
“It does help that a third of our population lives in Salt Lake County,” she said, adding that cases in other areas of the state continue to rise.
On Monday, Dr. Angela Dunn, epidemiologist with the Utah Department of Health, expressed optimism the state can reach the goal of reducing its seven-day rolling average but said it would take “a concerted effort over the next several weeks.”
Herbert’s office on Monday confirmed he is continuing to review data ahead of Saturday’s deadline and meeting to discuss Utah’s next move in the pandemic. Early in July, he warned that if Utah can’t decrease its rolling average to fewer than 500 cases by August, “it may trigger some more aggressive action by the government.” He has not said directly what that action might include.

New cases, hospitalizations
On Tuesday, 446 new cases were confirmed of 4,651 tests reported, with a 9.6% positive rate. They bring the state’s total since the pandemic began to 38,855 of 514,509 people tested — a 7.6% overall positive rate, according to the Utah Department of Health.
The largest increases in cases on Tuesday occurred in Salt Lake County, where 161 were confirmed; Utah County, with 126; Weber Morgan, with 52; Davis County, with 41; and Southwest Utah, with 33.
Nearly 26,000 of the state’s cases are considered recovered after passing the three-week point since their diagnoses.
Currently, 211 patients are hospitalized for COVID-19 in Utah, 83 of whom are in intensive care units. The state’s intensive care units — which have about 600 beds overall — are 59.3% full with coronavirus patients and others, while other hospital beds are 45.9% full.
Of Utah’s 2,295 COVID-19 hospitalizations since the pandemic began, 592 — or 25.8% — required care in intensive units, and 240 patients — or 10.5% — required ventilators, according to state data.
Even while experiencing its surge, Utah’s hospitals haven’t reached the point where they’ve become overwhelmed, although leaders from the biggest hospital systems have warned that they could become so if the surge continues. But a new analysis out of George Washington University’s Milken Institute of Public Health found that Utah is one of 11 states that could face a shortage of doctors trained to work in intensive care units.
“This week’s update shows that Alabama, Arkansas, Florida, Idaho, Louisiana, Mississippi, Nevada, Oklahoma, South Carolina, Utah and Washington all could face a shortage of intensivists. In these states, less than 50% of intensivists are available for non-COVID patients,” said Patricia Pittman, director of the Milken Institute, in a statement.
“Arizona and Texas face a shortfall of intensivists even just for the COVID-19 patients. Our estimator suggests that a rapid increase in severely ill COVID-19 patients could overwhelm understaffed ICUs in many states,” she said.
Utah has 81 intensivists — doctors trained to work in intensive care units. The researchers say that’s an adequate supply at average demand for care, but Utah could face a shortfall if a larger surge in cases occurs, as the University of Washington’s Institute of Health Metrics projects.
But Keegan said that, due to the difficulty in projecting the disease so far, her team isn’t attempting to predict what could happen in November.
“There’s so many possibilities that trying to project out what’s going to happen in November, it’s unknowable at this point. ... What happens with COVID over the next few months or year is not just a factor of the disease epidemiology, it’s the interaction between the disease and our behavior,” Keegan said.
“What happens in November is dependent on behavior that we as a community are doing right now. Any reduction in cases is a good reduction in cases. Ideally, we would try to get it down to zero, but starting at below 500 seems like a really good place to start,” she said.

5 more deaths reported
The latest deaths were a Salt Lake County man older than 85 and a Washington County woman between 65-84, both of whom were hospitalized when they died. Three long-term care residents also died from complications due to the disease: a San Juan County man older than 85; a Davis County woman between 65-84, and a Salt Lake County man between 65-84.
They bring the state’s death toll from the novel coronavirus to 286. Of them, 90.6% were considered at high risk, meaning they were at least 65 years old and/or had underlying health conditions. Just under 130 deaths were residents in long-term care facilities.
Utah’s death rate of confirmed cases now stands at about 0.74%.
The latest breakdown of Utah cases, hospitalizations and deaths by health district:
- Salt Lake County, 18,441; 1,199 hospitalized; 162 deaths.
- Utah County, 7,422; 348 hospitalized; 31 deaths.
- Southwest Utah, 2,814; 152 hospitalized; 24 deaths.
- Davis County, 2,784; 159 hospitalized; 12 deaths.
- Weber-Morgan, 2,427; 150 hospitalized; 24 deaths.
- Bear River (Box Elder, Cache, Rich), 2,105; 85 hospitalized; 5 deaths.
- Summit County, 673; 52 hospitalized; 1 death.
- San Juan County, 591; 75 hospitalized; 22 deaths.
- Wasatch County, 519; 20 hospitalized; 4 deaths.
- Tooele County, 511; 23 hospitalized; 0 deaths.
- Central Utah, 353; 19 hospitalized; 1 death.
- TriCounty (Uinta Basin), 144; 8 hospitalized; 0 deaths.
- Southeast Utah, 71; 5 hospitalized; 0 deaths.


