SALT LAKE CITY — While hospitals across Utah and the United States are seeing plenty of COVID-19 patients, it’s a dearth of other patients that is becoming a concern.
People seem to be delaying necessary treatments because of a fear that hospitals might be contaminated with the virus, Gov. Gary Herbert said during his weekly COVID-19 briefing on Thursday.
“That’s a false fear,” he said.
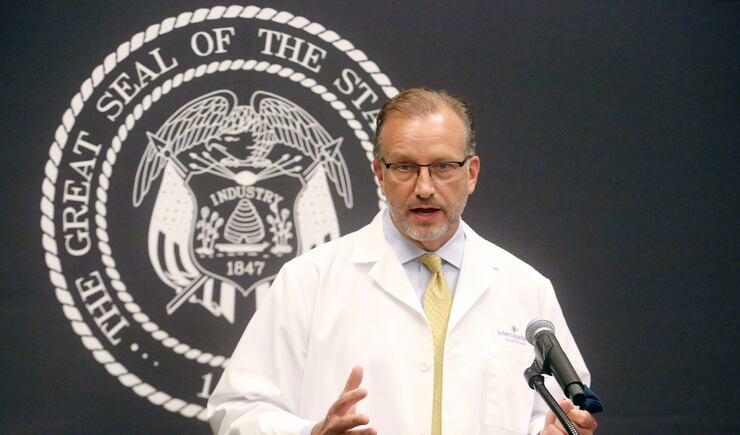
Dr. Mark Briesacher, chief physician executive at Intermountain Healthcare, said Intermountain hospitals, as well as others, are seeing a 40% reduction in patients coming to the hospital with symptoms of stroke and 35% fewer with symptoms of heart attack, as well as other emergent and potentially life-threatening conditions.
“In these conditions, every minute counts,” he said, encouraging anyone with any type of medical condition to ensure they’re getting the treatment they need. “Our hospitals are safe and they are ready for any health care need that you have.”
In addition to providers wearing masks, shields and gowns, Briesacher said hospitals have designated areas where COVID-19 patients are treated, as well as devices that purify the air. He said hospitals are always doing everything they can to prevent infection and cross-contamination and, during a pandemic, it is no different.
“It’s really important that you don’t delay care. It’s important for your health and for our community’s health. And, delays in care can actually be life-threatening,” he said. “If you’re due for a skin cancer screening, breast cancer screening, colon cancer screening, please go and get that done.”
Earlier this year, hospitals asked that people delay elective procedures whenever possible, but have never limited their capacities for emergent care. Currently, about 54% of all hospital beds are being used, and only a small portion of those are patients being treated for symptoms of COVID-19, according to Utah Department of Health data.

Another 334 newly confirmed cases of COVID-19 were reported in Utah on Thursday, as well as two new deaths resulting from the disease.
The rolling seven-day average daily number of cases is 354 and the seven-day average test positivity rate is 8.6%. A week ago, it was closer to 10%.
Utah now has a total of 45,424 COVID-19 cases caused by the novel coronavirus, which began circling the globe in February.
The latest two deaths include a Salt Lake County man between the ages of 65 and 84 who was not hospitalized when he died, and a Salt Lake County woman, who was older than 85 years old and was a resident of a long-term health care facility when she died. The health department has said it is careful to ensure that deaths counted as COVID-19 fatalities in Utah are confirmed as deaths that would not have happened without COVID-19.
In all, 353 people in Utah have died because of the pandemic illness.
There are 184 people currently hospitalized in Utah hospitals, and 2,721 people, in all, have been hospitalized throughout the pandemic, which hit Utah in mid-March.
The state has tested 584,656 people for COVID-19, though the demand for testing has diminished in recent weeks.
“We believe there is less prevalence of disease in the state,” the health department’s Nathan Checketts, who is also serving as testing director with the state’s Unified Command, said on Thursday. He said testing sites across the state are reporting a 20% to 30% reduction in demand as infection rates have gone down, albeit slowly, according to daily reports.
Checketts spoke about the need for testing, which gives the state the information it needs to command its response.
“We have made tremendous efforts to get where we are today,” he said, adding that the state is now utilizing three different types of tests and is awaiting greater supply of antigen testing kits, which can identify current infection in about 15 minutes.
Anyone with symptoms is encouraged to seek out testing by calling a health care provider or getting a referral through the state’s coronavirus.utah.gov website. Checketts said most tests don’t cost patients anything and help to inform individuals, as well as their close contacts, whether isolation and quarantine are necessary to prevent the spread of disease.
The state has yet to expand its criteria for testing because health officials are cautiously awaiting the reopening of schools and the potential for widespread transmission of illness that could result, as well as the upcoming influenza season that could bring its own complications, Checketts said.
He said that with decreased demand, laboratories are turning out results more quickly, even within a day at the state’s public health laboratory.
The health department estimates that at least 35,817 people previously diagnosed with the virus have recovered. More information can be found online, at coronavirus.utah.gov.
“We’ve come a long way through this pandemic,” Herbert said, adding that he’s pleased with recent trends.
As schools open, he said Utahns will need to be patient as adjustments are made. Wearing masks, social distancing and proper hand washing will become even more important.
“It’s no time for us to be complacent,” Herbert said. “If anything, we need to increase our efforts.”
He said evidence points to schools being an important place for learning and development to take place. And, while a lot of work has gone into the various plans for operating Utah’s 41 school districts, Herbert said it could all be reversed if the virus starts to spread.
“There is no way to absolutely have zero risk,” he said. “There is risk involved. All plans have a Plan B in case it doesn’t work. If infections rise to unacceptable levels ... we will drop back to all distance learning like we did in the spring.”
The latest breakdown of Utah cases, hospitalizations and deaths by health district:
- Salt Lake County, 21,199; 1,386 hospitalized; 204 deaths.
- Utah County, 9,062; 428 hospitalized; 37 deaths.
- Davis County, 3,316; 188 hospitalized; 21 deaths.
- Southwest Utah, 3,264; 184 hospitalized; 26 deaths.
- Weber-Morgan, 2,935; 187 hospitalized; 25 deaths.
- Bear River (Box Elder, Cache, Rich), 2,358; 110 hospitalized; 7 deaths.
- Summit County, 718; 53 hospitalized; 1 death.
- San Juan County, 651; 87 hospitalized; 25 deaths.
- Tooele County, 598; 30 hospitalized; 0 deaths.
- Wasatch County, 584; 22 hospitalized; 4 deaths.
- Central Utah, 442; 25 hospitalized; 2 deaths.
- TriCounty (Uinta Basin), 183; 14 hospitalized; 0 deaths.
- Southeast Utah, 114; 7 hospitalized; 1 death.